
Approximately 80% of patients present with advanced disease, which is difficult to cure and is associated with short survival times 2. In the United States, pancreatic cancer is the 3 rd leading cause of cancer-related death 1. Recent medication changes should be considered as candidate features in multi-factor risk models for PDAC, though they are not causally implicated in development of PDAC. These changes are not associated with diagnosis of other digestive system cancers. Two-year PDAC risk increases as number of relevant medication changes increases ( P-trend <1 × 10 −5), with participants who recently start antidiabetic and stop antihypertensive medications having multivariable-adjusted hazard ratio of 4.86 (95%CI, 1.74–13.6). Here we show recent initiation of antidiabetic (NHS) or anticoagulant (NHS, HFS) medications and cessation of antihypertensive medications (NHS, HPFS) are associated with pancreatic cancer diagnosis in the next 2 years. participants followed for 2,994,057 person-years and 991 incident PDAC cases.
We investigate recent medication changes and PDAC diagnosis in Nurses’ Health Study (NHS females) and Health Professionals Follow-up Study (HPFS males), including up to 148,973 U.S.

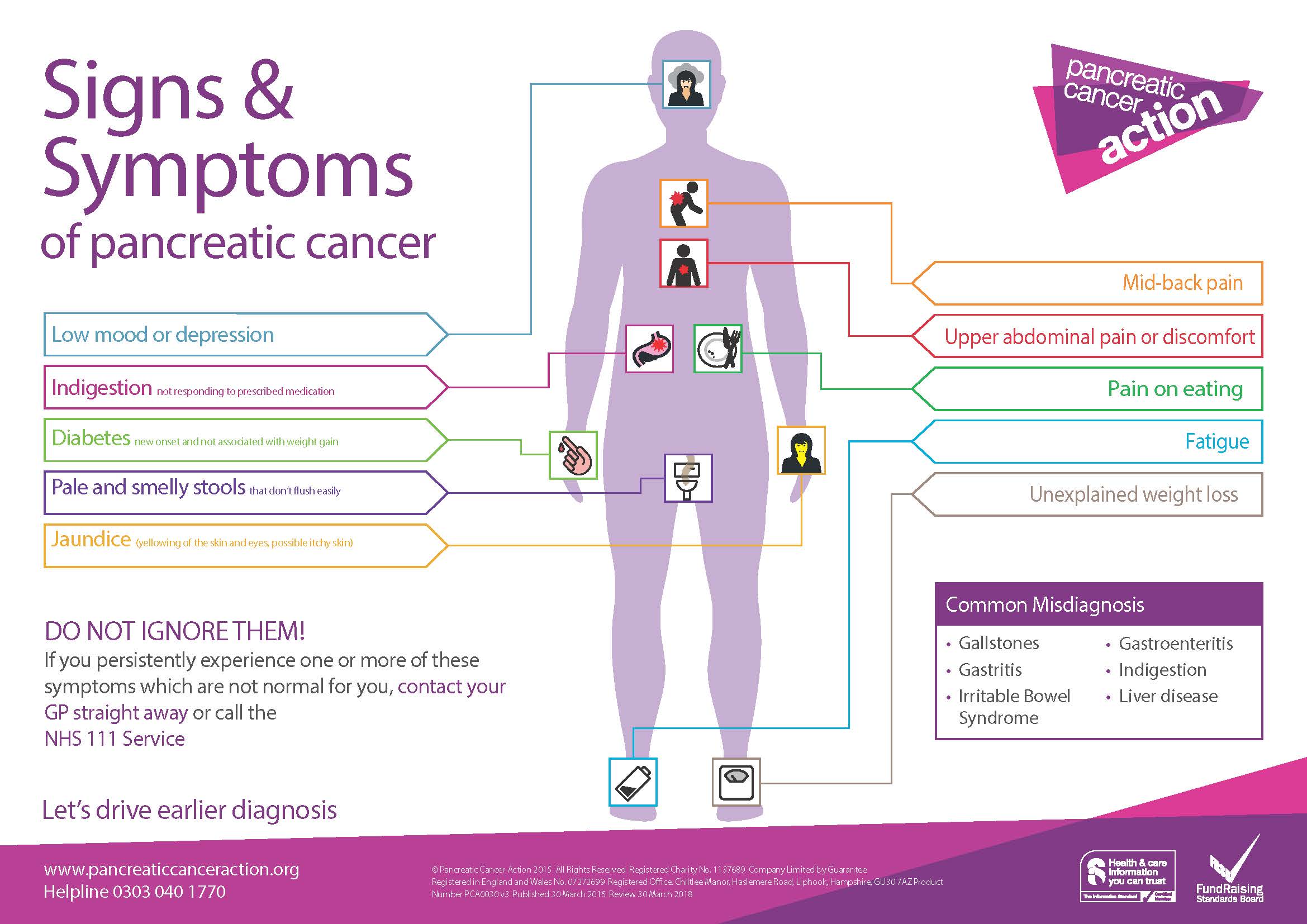
Patients with pancreatic ductal adenocarcinoma (PDAC) commonly develop symptoms and signs in the 1–2 years before diagnosis that can result in changes to medications.


 0 kommentar(er)
0 kommentar(er)
